-
Talk to Our Care Planner
In-Home Dementia Care Costs: What Families Pay and What to Expect in 2025

Caring for a loved one with dementia at home is a labor of love – and it can also be confusing and overwhelming, especially when it comes to costs.
You’re not alone if you’re asking, “How much will in-home memory care cost, and what should we budget for the future?” Many family caregivers reach a point of burnout.
In this guide, we’ll break down what families actually pay for in-home dementia care in 2025 and how to plan ahead.
TABLE OF CONTENT:
Quick Reference Cost Table – Home Care vs. Memory Care (National Averages)
| Care Option | Average Cost |
| In-Home Dementia Care | ~$33 per hour (national median). That’s about $5,000–$6,300 per month for a typical 40 hours/week of care. Part-time (15 hr/week) is around $2,145/mo, while 24/7 care can far exceed this range.
|
| Memory Care Facility (Residential) | ~$6,450 per month (national median) for specialized memory care in a community. Costs range widely (~$4,000 to $11,000+ monthly) depending on location and level of care.
|
Home care costs are usually charged by the hour, giving families flexibility. Memory care facility costs are typically charged per month as a package (housing, meals, care included).
It’s a good idea to check rates in your area, since costs in, say, rural areas vs. big cities can be as different as apples and oranges. You might be pleasantly surprised or (we’ll be honest) a bit shocked, but at least you’ll know what to expect.
Need to Talk to Memory Care Planner for Counsel?

What Is In-Home Memory and Dementia Care?
In-home memory care means bringing trained caregivers into your loved one’s home to help with daily tasks and keep them safe, happy, and healthy. “Memory care” and “dementia care” are terms often used hand-in-hand.
The difference is mostly in how and where care is provided:
-
Dementia Care:
This is a broad term for caring for someone with dementia at any stage, in any setting. It can be provided at home, in adult day centers, in assisted living, or in nursing facilities – basically anywhere support is given to a person with memory loss.
-
Memory Care:
This usually refers to a specialized care setting – often a dedicated wing of an assisted living or nursing home, or a standalone community, designed just for people with Alzheimer’s or other dementias.
Memory care facilities have secured environments (to prevent wandering), staff trained in dementia, and structured activities for residents. Think of memory care as a type of dementia care that’s facility-based and highly specialized for memory issues.
To better understand both terms and what each involves, you can explore our detailed explanation of dementia and Alzheimer’s care.
Comparison of Care Settings:
- In-Home Care:
Caregivers come to your house. The senior stays in their familiar environment. Care is one-on-one and personalized. Families often choose this to keep their loved one at home as long as it’s safe.
- Memory Care Unit (in Assisted Living or Nursing Home):
A secure residential unit with specially trained staff and programs for dementia. Residents live there full-time, receiving 24/7 supervision, meals, help with bathing, dressing, medication, and memory-focused activities. It’s a structured environment tailored to those with memory loss.
- Nursing Home:
A medical-based facility for those who need continuous skilled nursing care (e.g. they have other serious health issues). Some nursing homes have memory care units inside.
Nursing homes provide the highest level of care outside a hospital – including feeding tubes, injections, or therapy – things in-home care or standard memory care facilities usually can’t do. Nursing homes are also the most expensive care setting on average.
If you’re comparing those options, here’s a breakdown of assisted living vs nursing home differences.
What services does in-home memory care provide?
In-home dementia care services cover almost everything short of medical procedures. A professional in-home caregiver can help with:
- Personal Care: Bathing, grooming, using the toilet, and getting dressed (no more worrying if Dad forgot to change his shirt – the caregiver’s on it).
- Medication Management: Making sure pills are taken on time and the right way (because those schedules can get confusing!).
- Meals: Planning and cooking nutritious meals – and even feeding the person if needed.
- Mobility & Exercise: Helping your loved one move around safely, get in/out of bed or chairs, and maybe take gentle walks for exercise.
- Companionship: Providing friendly interaction, conversation, and activities to keep the senior engaged and less isolated. (Yes, this might include listening to Grandma’s stories again – caregivers are very patient!).
If you’re looking for meaningful ideas to keep your loved one mentally and emotionally stimulated, here’s a curated list of simple and powerful activities for seniors with dementia that can be done at home, even with early-stage memory loss
- Household Tasks: Light housekeeping, laundry, tidying up, and even grocery shopping or errands.
- Transportation: Driving or accompanying your loved one to doctor appointments or social outings. If you have senior with mobility issues, you may also want to consider these elderly bed exercises could provide great relief.
- Safety Supervision: Preventing wandering or unsafe behaviors and keeping an eye out to ensure the senior is okay at all times. This is crucial for dementia patients who might forget stove burners or get confused at night.
Essentially, in-home memory care tries to mirror what a memory care facility offers except it’s all happening in the comfort of home, one-on-one.
How Much Does In-Home Dementia Care Cost in 2025?
Let’s dig into the dollars and cents. How much does in-home memory care actually cost? The answer depends on how much care you need and where you live, but we’ll break down typical ranges.
Hourly rates: In-home dementia care is usually billed by the hour. In 2025, hourly rates range from about $20 to $40 per hour on average.
- The national median cost for a home health aide is around $33 per hour. That means half of providers charge less than that, half charge more.
- Rural or less expensive areas might be closer to the $20–$25/hour end. Big cities or regions with high living costs (and higher caregiver wages) tend toward $30–$40/hour.
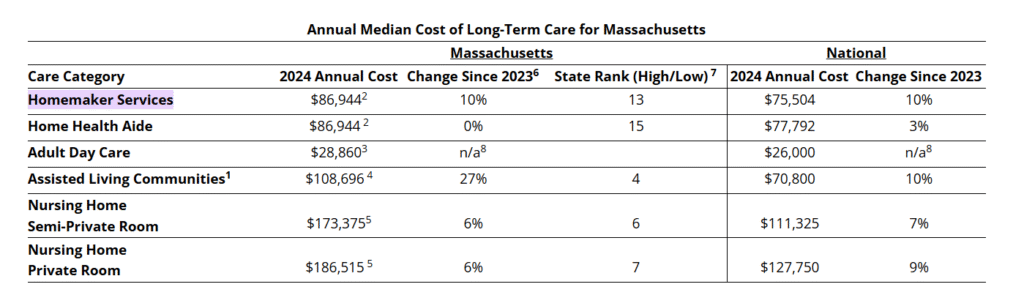
For instance, in Mississippi and Louisiana, home care can be as low as ~$23–$25/hour, whereas in states like Massachusetts or Minnesota it’s more common to see $35–$40+ per hour.
In Massachusetts, the typical rate is about $38/hour for in-home care – higher than the national average, reflecting the higher cost of living. You can check specific rates and agency options in the state of Massachusetts here.
Weekly & monthly averages: It helps to think in terms of how many hours of care per week your loved one needs. Here are some ballpark figures:
- Part-Time Care (e.g. 15 hours per week): About $2,100–$2,200 per month. This might be the case if you hire a caregiver for a few hours each weekday to help Mom with lunch, medication, and a walk, for example.
- Full-Time Daytime Care (40 hours/week): Around $6,000–$6,300 per month on average. Essentially, this is like paying for a full-time job’s worth of care (8 hours a day, 5 days a week).
- 24/7 Care: Now we’re in the big leagues of cost. If you truly need round-the-clock, 24-hour coverage at home, you will likely have multiple caregivers in shifts or a live-in with backups. This can run $10,000–$15,000+ per month in many cases.
(Some families report spending about $8,000–$10,000 a month for two live-in caregivers providing 24/7 care in Los Angeles. In high-cost areas or with agency rates, 24/7 home care can even exceed $15K monthly – more expensive than a nursing home, unfortunately.)
Why such a wide range? Price factors play a big role in what your unique situation will cost:
- Level of Care Needed:
The more advanced the dementia (more help with dressing, toileting, managing difficult behaviors, etc.), the more you may pay. Advanced care might require caregivers with specialized dementia training at a higher hourly rate.
- Number of Hours:
This one’s obvious – needing help 4 hours a day will cost much less than needing 16 hours a day. You pay for the caregiver’s time. Many agencies have minimum shifts (e.g. 2-4 hours). As needs increase, costs scale up accordingly.
- Location (Geography):
Costs in different states (even different cities) vary a lot. Wages and cost of living drive home care prices.
For example, Massachusetts home care costs exceed national averages, whereas some Southern and Midwestern states are more affordable. Always check your local area rates.
- Agency vs. Private Hire:
Hiring a caregiver through a home care agency often costs more per hour (maybe $5–$10 more) than hiring an independent caregiver. Agencies handle background checks, training, scheduling replacements if someone’s sick, and insurance – you pay for that convenience.
If you hire privately (like finding someone on your own), it can be cheaper, but be very careful to vet and consider tax/employment obligations.
- Caregiver’s Skills and Training:
A certified nursing assistant (CNA) or caregiver with years of dementia experience might charge more than someone new or untrained. Also, if medical tasks are needed (like wound care), you’d need a skilled home health aide or nurse, which costs more.
- Time of Day / Holidays:
Evening, overnight, or weekend care sometimes costs extra (like “nanny rates” higher after midnight, etc.). Agencies also charge 1.5x on holidays in many cases – yes, even caregivers deserve holiday pay.
All these factors mean in-home dementia care costs can vary a lot, but understanding them helps you budget.
On the bright side, in-home care is flexible – you can start with a few hours and increase as needed, or vice versa, to manage expenses. Many families creatively combine family caregiving with part-time paid care to balance both cost and quality care.
How does in-home memory care cost compare to other care options?
Here’s a quick comparison for perspective:
- In-Home Care:
Around $20–$40/hour as discussed (roughly $3K–$6K per month for moderate schedules, more for 24/7).
- Assisted Living Facility:
Assisted living (for seniors who need help but not 24/7 nursing) costs about $5,900 per month on average in 2024. This typically includes housing, meals, and basic personal care.
Note: Standard assisted living may not be equipped for advanced dementia, though some have memory care units.
- Memory Care Facility:
Memory care usually costs about 20% more than assisted living. The national median is ~$6,450 per month in 2025. We often see memory care prices ranging from roughly $4,000 up to $8,000+ a month, depending on the state and facility amenities.
For instance, a memory care community in a small town might charge $4,500, whereas a fancy one in Boston or San Francisco suburb could be $10,000+.
- Nursing Home:
A nursing home is the priciest option because it provides full medical care. The average nursing home costs about $9,300 per month for a semi-private room, or $10,600 per month for a private room (national median).
In Massachusetts, nursing homes are even higher – easily $14,000–$15,000 per month for a private room. Ouch!
So, if your loved one only needs, say, 6 hours of help a day, in-home care could be far cheaper than moving them to a facility.
On the other hand, if 24-hour supervision becomes necessary, families often find the monthly cost of in-home care may equal or exceed facility costs. It’s a balancing act between the person’s needs, quality of life, and budget constraints.
When is in-home dementia care appropriate?
In-home dementia care is often best in the earlier to mid stages of Alzheimer’s or dementia – when your loved one needs some help and supervision but doesn’t require intensive medical interventions.
If your family can manage part of the care and just needs a few hours of help each day (for respite or specific tasks), in-home care is a wonderful choice. It lets the person stay in a familiar environment, which can reduce confusion and anxiety.
If you’re in that situation, this guide on how respite care helps explains how short-term care solutions support family caregivers.
For example, if Dad is mostly okay but forgetful, and just needs someone to make meals, ensure he bathes, and keep him company while you’re at work – in-home care a few hours a day could be perfect.
If you’re looking for sample caregiver routines that are best suited for managing early stages of memory loss, take a look at our sample daily schedule for elderly loved ones.
Staying at home is often appropriate as long as it’s safe: the home can be adapted for dementia (locks, alarms, removing trip hazards), and the person isn’t at high risk of hurting themselves or others.
However, as dementia progresses, the care needs grow. There may come a time when 24/7 supervision or medical care is needed that is hard to provide at home (we’ll talk about signs of that in a bit).
When to Move From In-Home Care to a Memory Care Facility

How do you know it’s “time” to consider moving your loved one out of the home and into a memory care community or unit? This is one of the hardest decisions families face.
There’s no single right answer, but there are common signs that it may be time to transition from in-home care (or regular assisted living) to a more intensive memory care setting. Here are a few big ones:
-
Increasingly Unsafe at Home:
If despite in-home help and safety modifications, your loved one is doing things that put them in danger – for example, leaving the stove on, wandering out the door and getting lost, or frequently falling – it might be time for a secured memory care environment.
Safety is paramount. Memory care facilities are designed to prevent injuries and wandering-related incidents.
-
Care Needs Exceed What Family/In-Home Aides Can Provide:
Perhaps your relative now needs constant supervision and help with almost everything 24/7. Maybe they’re up multiple times a night and you cannot keep a caregiver around the clock or cover nights yourself.
When everyday routines (bathing, dressing, toileting, eating) become unmanageable at home, a facility with 24-hour staff can meet those needs.
-
Worsening Behavior or Mood Changes:
Dementia can bring on agitation, aggression, extreme confusion, or even hallucinations. If your loved one is becoming very disoriented, wandering into unsafe areas, or showing aggressive outbursts that are hard to handle at home, professionals in memory care are trained to manage these behaviors in a safe environment.
For example, if Grandpa started having combative behavior due to sundowning that puts you or him at risk, a memory care facility can ensure he and others stay safe.
-
Decline in Personal Hygiene or Health:
Perhaps you notice Mom isn’t bathing or changing clothes, or she’s not taking her medications correctly even with reminders. In a memory care setting, staff will make sure she stays on top of hygiene and meds.
If in-home care can’t sufficiently keep up with these needs (for instance, if Mom resists the in-home caregiver’s help), a facility might be able to enforce a routine better.
-
Caregiver Burnout or Family Strain:
Let’s talk about you, the caregiver. Are you exhausted, stressed, or neglecting your own health? If caring for your loved one at home (even with hired help) is causing you significant burnout or impacting your physical/mental health, it’s a serious sign that a change is needed.
This honest piece about feeling trapped while caregiving may speak to your experience and help guide your next step.
A memory care facility can provide relief – you’ll always be their family, but you don’t have to be on duty 24/7. There’s no shame in admitting you need help; in fact, recognizing your limits is incredibly important.
As one source puts it, if you feel your own health is suffering or you’re burnt out, transitioning to memory care can provide peace of mind for everyone.
-
Emotional signs are valid too:
Trust your gut. If you’re constantly anxious about your loved one’s well-being when you’re not watching them – for example, you can’t sleep at night because you worry, they might wander or fall – that stress is telling you something.
Families often say, “I promised I’d never put them in a home,” which is heartfelt, but remember, a quality memory care home might actually provide the safety and specialized care that keeps your loved one healthy (and can prolong their life and comfort).
You’re not “giving up” – you’re choosing the best care environment for the stage of the disease.
One caregiver summarized it well:
“Someone with dementia should go into memory care if their safety is at risk and their needs are no longer being met at home… If you’re struggling to keep up, or your own health is suffering, the right memory care facility can provide peace of mind.”
Benefits of In-Home Dementia Care vs. Facilities

Both options have pros and cons. Since we’ve talked a lot about facilities, let’s highlight some big benefits of in-home dementia care (because there are many!):
-
Personalized, One-on-One Care:
At home, your loved one gets undivided attention. A caregiver is solely focused on them during their shift, rather than dividing time among multiple residents. This means care can be truly tailored to your family member’s personality, likes, and dislikes.
If Grandpa loves a particular TV show each afternoon, an in-home aide can make that part of the routine. If Grandma hates broccoli, the caregiver won’t put it on her plate. It’s very customized. In contrast, in a facility even the best staff have to split attention among several residents.
-
Familiar, Calming Environment:
There’s no place like home, especially for someone with dementia. Being in their own home – surrounded by familiar furniture, photos, and neighbors – can reduce confusion and anxiety that often come with being in strange new places.
Memory care patients thrive on familiarity. The home environment means they don’t have to adjust to a new setting, which can be scary and disorienting for them.
As one caregiving organization put it, “In-home memory care offers a familiar, calming environment that helps reduce confusion and anxiety for dementia patients.”
There’s comfort in sleeping in your own bed, hearing your own kitchen noises, and seeing your pet cat on the windowsill – little things that a facility can’t replicate.
And for ideas to enrich this home-based care environment, look through some of our best recommended home activities for seniors with dementia.
-
Flexibility and Routine on Your Terms:
In-home care can start slow or ramp up as needed. You control the schedule. Need someone just in the mornings for now? Sure. Later, need to add evenings? Can do.
This flexibility is a huge perk. Plus, your loved one can maintain their usual daily routine much more easily at home. Want to have lunch at 11 am instead of 12? Go for it.
Prefer bathing at night instead of morning? Fine. Facilities have set schedules to manage many people at once; at home, your loved one’s schedule is the priority.
-
Family Involvement and Peace of Mind:
With in-home care, you and other family members can be as involved as you want. You’re literally on home turf, so you can easily drop in, monitor the quality of care, and continue helping out without the burden all falling on you.
Caregivers work with the seniors to find the best daily activity plan based on an elderly caregiving checklist defined by your family.
Many families appreciate being able to spend quality time as family, not just as caregivers, when a professional is there handling the hard parts. You can share a cup of tea with Mom while the caregiver does the laundry, for instance.
Also, families often feel peace of mind knowing their loved one is in a familiar safe place and not among strangers.
There’s a sense of comfort when home doesn’t change. And if you have a multi-generational household, the grandkids or pets can still interact with Grandpa daily, which can be heartwarming for everyone.
-
Maintained Independence and Dignity:
Staying at home often allows seniors to keep a greater sense of independence. Even with a caregiver’s help, they’re in their domain.
They can decide if they want to sit on the porch or watch a specific TV program – it’s more of a one-on-one partnership than being one of many in a structured facility routine. This can preserve a sense of dignity and normalcy. They’re home, not “in a home.”
Need to Talk to Memory Care Planner for Counsel?

How to Pay for In-Home Dementia and Memory Care
How do families afford this?” Take a deep breath. There are several potential payment sources and strategies to explore. We’ll go over the big ones here:
1. Personal Savings and Income (Private Pay):
The reality today is that many families pay for care out-of-pocket at first. This means using the senior’s savings, pension, Social Security income, retirement accounts, or help from family members.
Here’s how families cover facility or home care using Social Security and other support programs.
If your loved one has a nest egg or assets (like a home), those often get tapped to cover care costs. Some people even take out a reverse mortgage to get cash from their home’s equity to pay for in-home care.
If you’re still in the early stages of planning, use this checklist of essential questions to start sensitive but necessary conversations about future care.
2. Long-Term Care Insurance:
Did your loved one purchase a long-term care (LTC) insurance policy in the past? If so, good news – these policies often cover both in-home care and memory care facility costs, up to the policy’s limits.
Every policy is different, so you’ll need to check the details (daily or monthly benefit amounts, maximum lifetime payout, elimination period, etc.). LTC insurance benefits can reimburse for a certain number of home care hours or pay a chunk of facility costs
3. Medicare (and Health Insurance):
A big question folks ask is, “Doesn’t Medicare cover any of this?” Medicare is the federal health insurance for people 65+, but it does not cover long-term custodial care.
That means Medicare will not pay for ongoing in-home caregivers or assisted living/memory care facility room and board. Medicare’s focus is on medical treatment, not personal daily care.
4. Medicaid:
Medicaid is the state-run insurance program for those with low income and assets.
It is the largest payer of long-term care in the U.S., but you have to qualify financially (which often means spending down assets to a few thousand dollars.
Real Family Scenarios & Cost Examples

Sometimes the best way to understand the costs is through real-life examples. Here is a real family scenario (gathered from caregivers’ stories online and in forums) that illustrates different care arrangements and what they paid.
Family #1 – Part-Time In-Home Care for Early-Stage Dementia:
“Grandma at Home with a Helper” – One family’s grandmother was in the early stage of Alzheimer’s. She could manage many things but was not safe to be alone all day.
The family hired an in-home caregiver through a local service for 4 hours each weekday (lunchtime through afternoon) mainly for supervision, meal prep, and companionship. This totals ~20 hours a week. They live in a mid-cost area.
Cost: About $2,500 per month for these part-time home care hours. (In their case, they found a caregiver who spoke Grandma’s native language, which was a big plus. At ~$2.5K/month, the family remarked it was an “incredible deal” – indeed, that works out to roughly $30/hour, which is on the lower side for their city.)
To see if this model fits your needs, review our guide on 24/7 in-home care costs.
This schedule allowed Grandma to remain at home with her routines. Her daughter handled mornings and evenings, and the paid caregiver covered mid-day. For over a year, this arrangement worked well and was more affordable than any facility.
It gave the family peace of mind that someone was checking in daily, without the cost of round-the-clock care.
Dr. Ella Njike is the branch administrator for Global One Home Care, Boston, an agency that provides quality care for seniors and kids or adults with disabilities. With a Doctorate and extensive experience working in the healthcare industry, Dr Ella brings a unique understanding to the challenges families face. Through Global One Home Care Boston, he ensures that care extends beyond daily tasks, focuses on building genuine connections and respecting each family's journey.
Contact us
We aim to be an active partner in your care, not to take over. You are the CEO of your care, and we support you in managing it effectively.
Here are some features of our Global One Home Care
- 24/7 access to care
- Customized care plans
- Supervisory visits
- Caregiver introductions
- Nutritional planning
- Respite support
- Companionship
- Mobility assistance
- Durable Medical Equipment recommendations
- Errands and Shopping
- Fall Prevention
- ADLs
