-
Talk to Our Care Planner
Dementia statistics in the United States 2025
Dementia is a significant health challenge across the United States, impacting millions of lives and placing a substantial burden on healthcare systems and families.
This blog post shines a light on recent dementia statistics in the United States, gathered from reputable official sources and published studies, offering clear explanations to help you understand the prevalence of dementia and its broader implications.
Here are the most important statistics on Dementia in the US in 2025.
Prevalence Of Dementia in The United States In 2025: The Numbers
These numbers surround Alzheimer’s and other forms of dementia, covering aspects from diagnosis rates and demographics to caregiving and costs. For detailed analysis on the broader industry, explore home health industry trends.
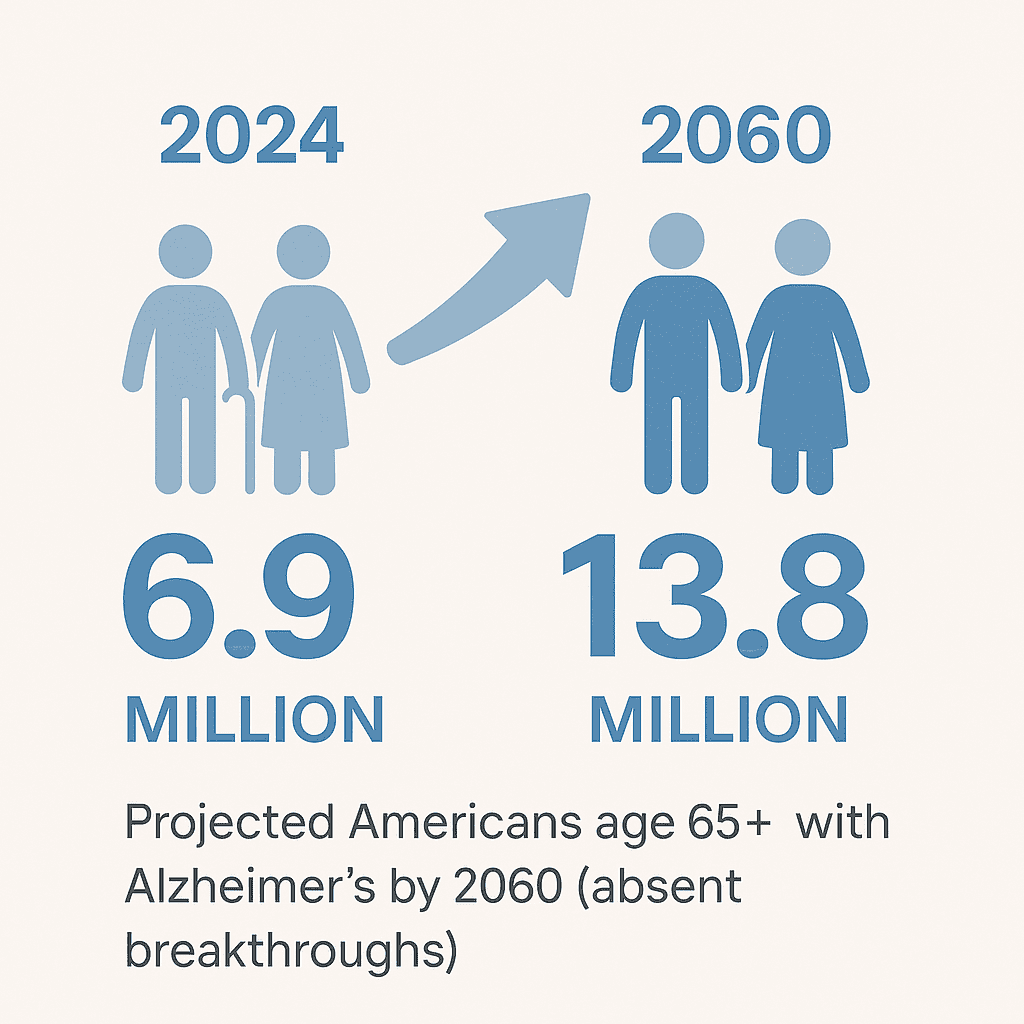
1. Older Americans Living with Alzheimer’s
6.9 million – Estimated number of Americans age 65 and older living with Alzheimer’s dementia in 2024.
This figure is up from 6.7 million in 2023, showing that dementia prevalence in US is on the rise, affecting more seniors each year.
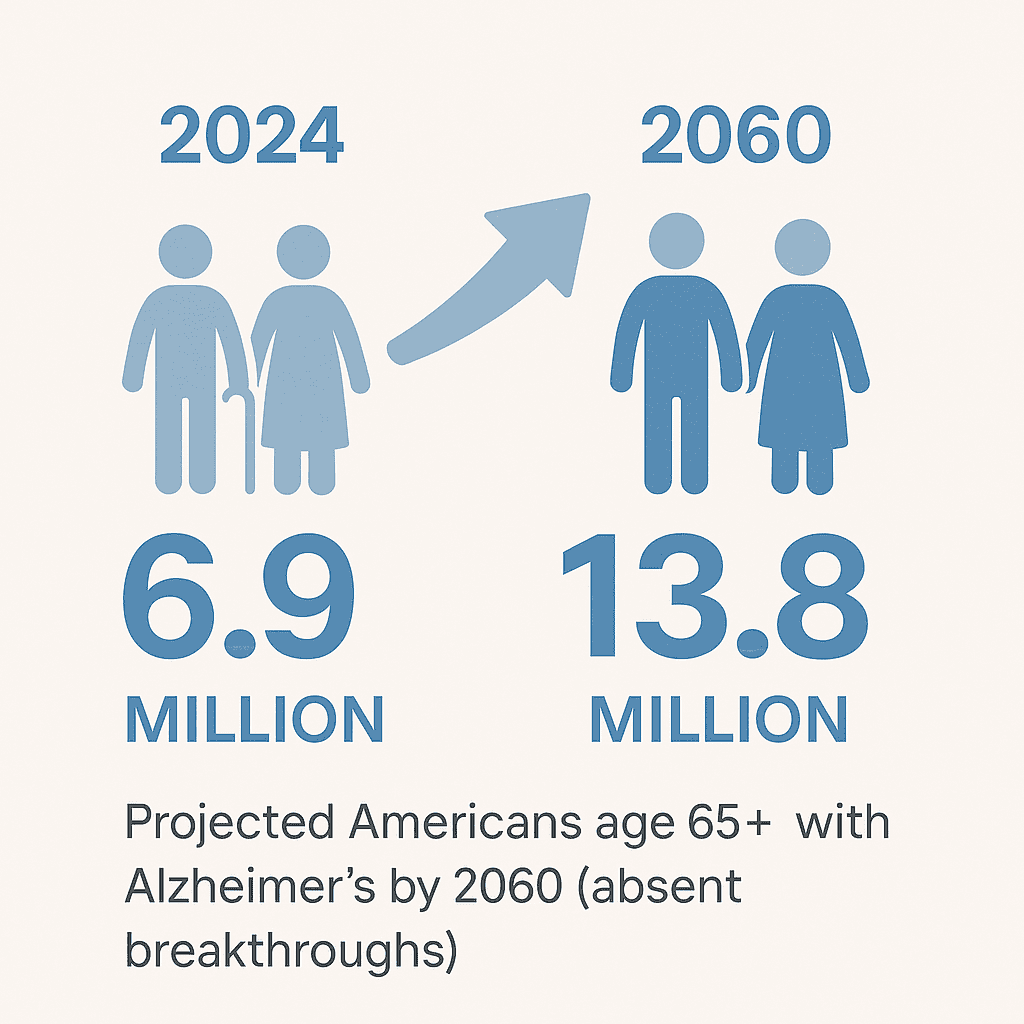
2. Projected Future Dementia Cases
13.8 million by 2060 – Projected population of Americans age 65+ with Alzheimer’s dementia by the year 2060, absent medical breakthroughs.
Looking ahead, experts believe the number of older Americans with Alzheimer’s could almost double by 2060 if new ways to prevent or cure the disease aren’t found. The aging Baby Boomer generation is the main driver behind this big jump in dementia in the United States, creating an urgent need for more resources.
3. Dementia in Massachusetts Seniors
135,200 (11.3%) in Massachusetts – Approximate number of Massachusetts residents age 65+ living with Alzheimer’s in 2020. Even at a state level, like right here in Massachusetts, Alzheimer’s is making a big impact.
More than one in ten seniors in our state are affected by this disease, making it a significant local health concern.
4. Age and Dementia Risk
Dementia risk rises with age: About 5% of Americans aged 65–74 have Alzheimer’s dementia, increasing to 13% for ages 75–84, and about 33% (1 in 3) of those 85 or older have Alzheimer’s.
As people age, their chances of developing Alzheimer’s dementia climb significantly. Being older is the strongest factor making someone more likely to get dementia.
5. Women and Alzheimer’s
Nearly 2⁄3 are women – Almost two-thirds of Americans living with Alzheimer’s are women. It’s an important fact that most people living with Alzheimer’s are women.
This could be because women generally live longer, giving the disease more time to develop, or perhaps due to higher biological susceptibility.
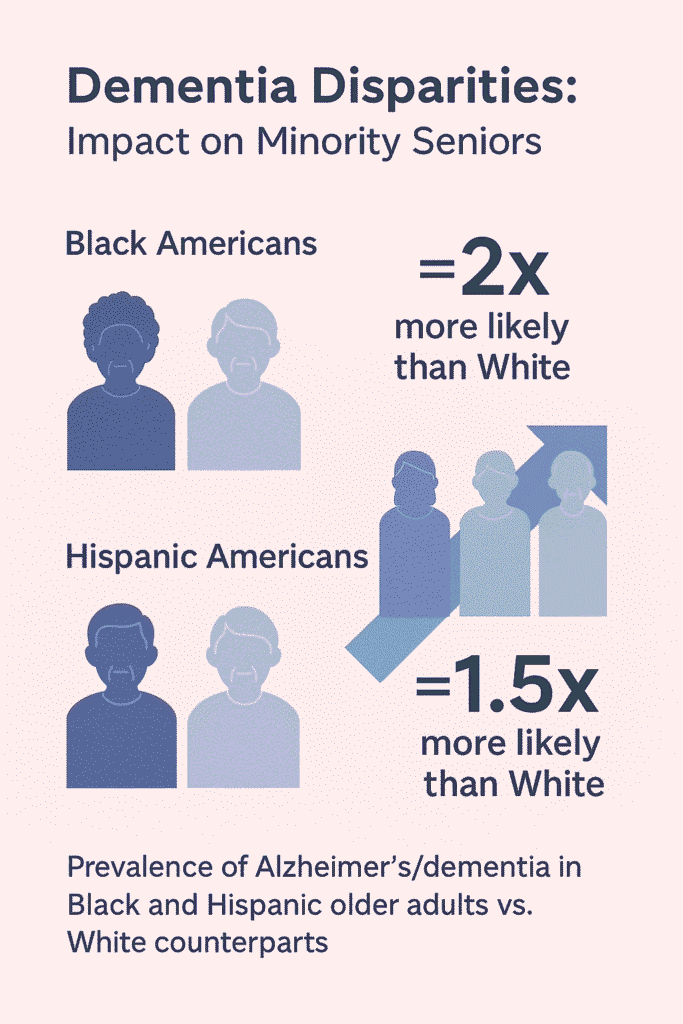
6. Disparities in Dementia Prevalence
Higher prevalence in Black and Hispanic seniors: Older Black Americans are about twice as likely as older White Americans to have Alzheimer’s or other dementias, and older Hispanic Americans are about 1.5× as likely as Whites to have these diseases. These figures show a clear difference in who is affected by dementia.
Older Black and Hispanic Americans face a higher risk, which can stem from different risk factors, unequal access to healthcare, and other parts of daily life that affect health. We Americans need to understand these disparities to tackle the overall statistics of dementia in the United States.
7. Younger-Onset Dementia Cases
~200,000 under 65 – An estimated 200,000 Americans under age 65 are living with younger-onset Alzheimer’s or other dementia.
While we often link dementia with older age, it also impacts younger adults. This figure reveals that a good number of people in their 30s, 40s, and 50s are living with younger-onset dementia, though such early-onset cases are less common.
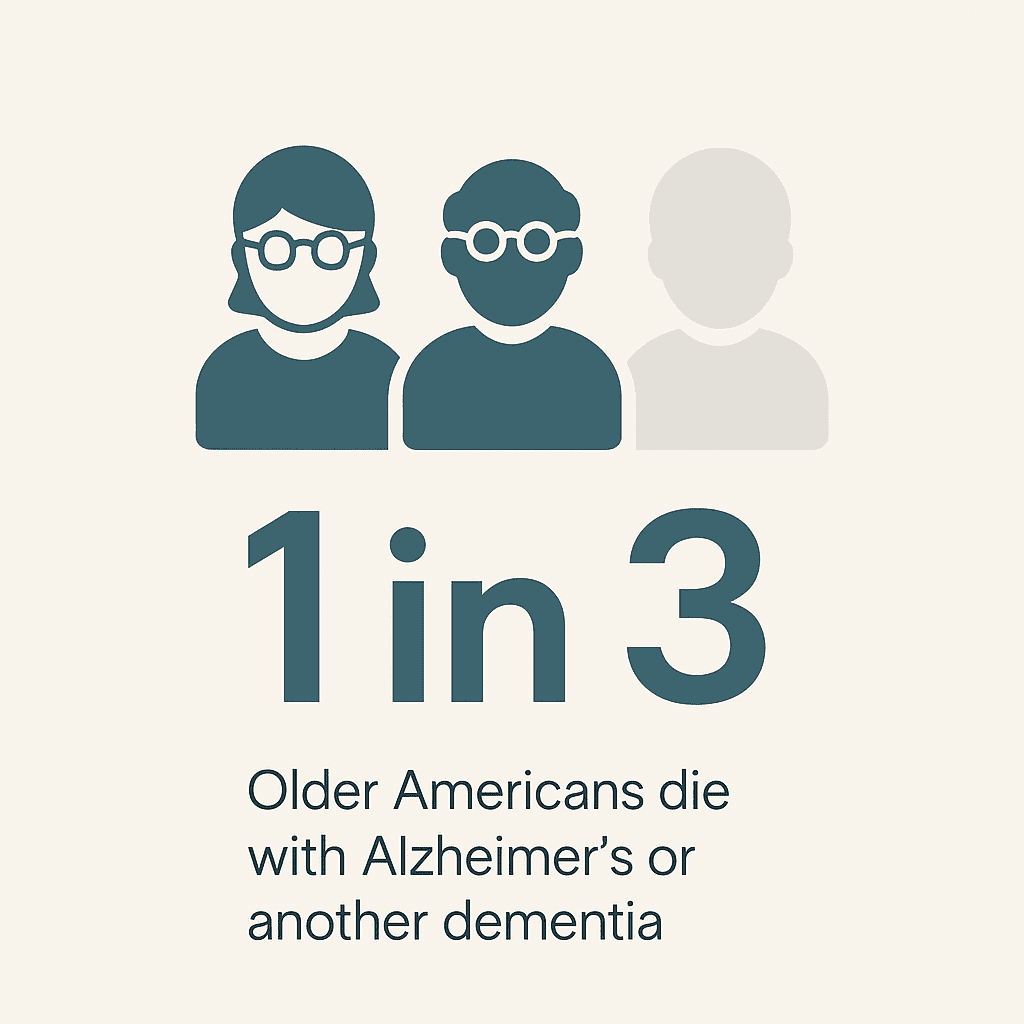
8. Dementia and Senior Mortality
1 in 3 seniors dies with dementia – Approximately one in three older Americans dies with Alzheimer’s disease or another dementia.
Alzheimer’s is a deadly disease. It causes more deaths than breast cancer and prostate cancer combined, underscoring its profound impact on the health of older adults.
9. Alzheimer’s as a Leading Cause of Death
7th leading cause of death (U.S.) – In 2021, Alzheimer’s disease was the 7th-leading cause of death in the United States, and it remains the 5th-leading cause of death among Americans age 65 or older.
Alzheimer’s disease ranks among the top reasons people die in our country, especially for those aged 65 and above. This places it alongside other major health conditions as a leading cause of death.
10. Alzheimer’s Deaths in Massachusetts
7th leading cause in Massachusetts – In Massachusetts, Alzheimer’s disease is also the 7th-leading cause of death, with 1,596 recorded Alzheimer’s deaths in 2022.
Following national trends, Alzheimer’s disease is also a major cause of death here in Massachusetts. The challenges and tolls of dementia are clearly felt at the local level.
11. Increase in Alzheimer’s Deaths
>140% increase in deaths – Between 2000 and 2021, annual reported deaths from Alzheimer’s disease in the U.S. surged by over 140%. This number is striking because it highlights how quickly the number of deaths from Alzheimer’s has grown in two decades.
In contrast, deaths from many other major diseases have actually gone down, underscoring the unique and increasing challenge Alzheimer’s presents.
12. Survival After Diagnosis
4–8 year survival after diagnosis – People age 65 and older survive an average of 4 to 8 years after an Alzheimer’s diagnosis, although some live up to 20 years with the disease. After an Alzheimer’s diagnosis, most people live for several years, though some can live much longer.
The disease slowly gets worse over time, and how long someone lives with it can vary greatly.
13. Increased Hospital Stays for Dementia Patients
Twice as many hospital stays – Older adults with Alzheimer’s or other dementias have roughly 2× the number of hospital stays per year compared to other seniors. Seniors with dementia spend much more time in the hospital than other seniors.
This often happens because they face more health problems like falls or infections, or they have more difficulty managing other chronic illnesses.
14. Preventable Hospitalizations
Preventable hospitalizations: Nearly 1 in 4 people with dementia has a hospitalization that is considered preventable with optimal care.
Many hospital visits for people with dementia could be avoided. Better overall management of their medical conditions and more support for caregivers could prevent many of these trips to the hospital.
15. High Hospice Utilization
High hospice usage – Alzheimer’s and other dementias are common at end-of-life: about 45% of all hospice patients in 2020 had a primary diagnosis of Alzheimer’s or another dementia. Dementia, especially Alzheimer’s, is a very common reason for people to receive hospice care at the end of their lives.
It’s second only to cancer as a reason for hospice for Medicare beneficiaries. For those navigating the complexities of dementia, specialized dementia support is available. This understanding of condition progression helps families plan for comprehensive care.
16. Total Annual Cost of Dementia Care
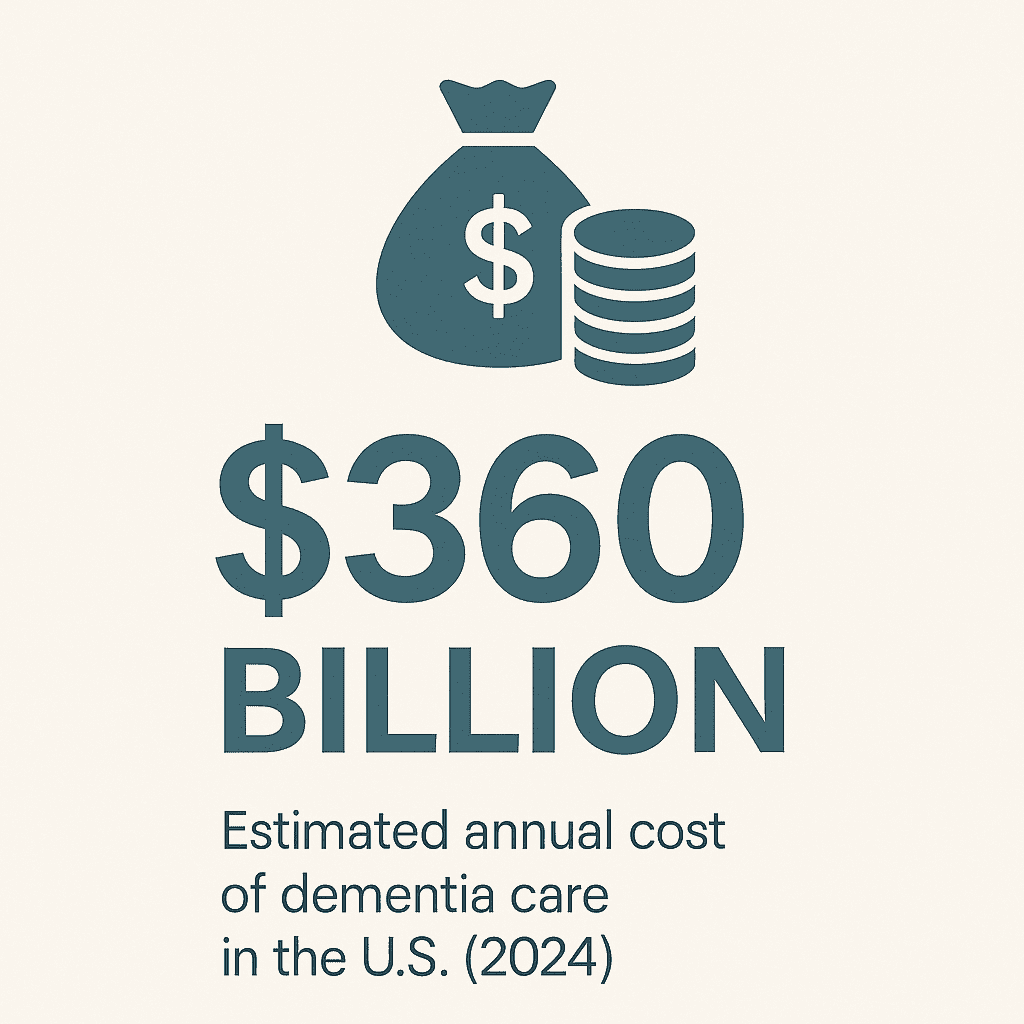
$360 billion – The total annual cost of caring for people with Alzheimer’s and other dementias in the U.S. is estimated at $360 billion in 2024. The cost of caring for people with dementia in the U.S. each year is incredibly high.
This massive number includes expenses for medical care, long-term care facilities, and hospice, but doesn’t even count the care provided for free by family members. This huge financial burden showcases the economic impact of the prevalence of dementia in us.
17. Rising Future Dementia Costs
Soaring future costs: U.S. dementia care costs are projected to reach $384 billion in 2025 and nearly $1 trillion by 2050.
Money spent on dementia care is expected to keep climbing rapidly. This huge increase is mainly because more people will get older, which means more people will need dementia care. Finding new ways to prevent or treat the disease is essential to control these skyrocketing costs.
18. Who Pays for Dementia Care
Medicare/Medicaid vs. out-of-pocket: Of the 2025 projected dementia costs, Medicare and Medicaid will cover about $246 billion (≈64%), while out-of-pocket spending by patients and families will total about $97 billion.
Government programs like Medicare and Medicaid pay for a large portion of dementia care costs. However, patients and their families still have to pay a very large amount directly out of their own pockets, which can create a huge financial struggle.
19. Lifetime Cost of Dementia Care
$405,000 per person – The average lifetime cost of care for a single person with dementia is estimated at $405,000 (in 2023 dollars). Caring for one person with dementia throughout their lifetime can cost a staggering amount of money.
Most of this cost, about 70%, falls directly on families, either through direct payments or the value of the unpaid care they provide.
While average lifetime costs are significant, daily in-home care costs, especially for 24/7 support, also factor into the overall financial picture for families. Many families eventually consider continuous elder care to ensure safety and comfort. This comprehensive assistance provides peace of mind around the clock.
20. Increased Healthcare Spending for Dementia
Higher healthcare spending: Annual Medicaid spending for an older adult with dementia is 22× higher than for one without dementia, and Medicare spending is about 3× higher for seniors with dementia versus those without.
These numbers clearly show how much more healthcare money is spent on seniors who have dementia. They use more services like nursing homes and medications, which significantly drives up the costs per patient.
21. Massachusetts Medicaid Spending on Alzheimer’s
$2.2 billion (MassHealth) – Massachusetts’s Medicaid program is projected to spend $2.2 billion in 2025 on care for people with Alzheimer’s disease.
Massachusetts’s Medicaid program, known as MassHealth, is expected to spend a huge amount of money specifically on Alzheimer’s care. This reflects a steady rise in spending and highlights the financial strain on state resources due to dementia statistics us.
22. Unpaid Dementia Caregivers
11+ million caregivers – Nearly 12 million Americans are unpaid caregivers for someone with Alzheimer’s or another dementia. A massive number of Americans are stepping up to care for family members or friends with dementia without getting paid.
These family members and friends provide essential help with daily activities, medical tasks, and supervision. Unpaid caregivers often assist with daily activities that fall under personal care services, such as bathing, dressing, and grooming. These services are fundamental to maintaining dignity and hygiene.
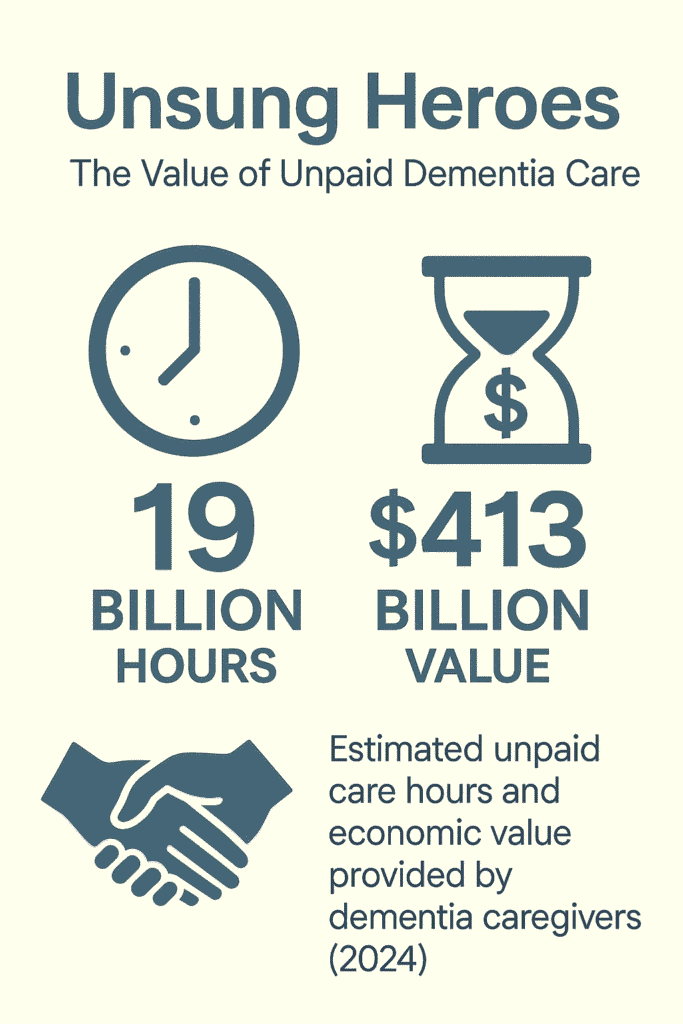
23. Value of Unpaid Caregiving
19 billion hours, $413 billion value – In 2024, unpaid dementia caregivers provided an estimated 19 billion hours of care, equivalent to over $413 billion in economic value. The amount of care provided by unpaid caregivers is truly incredible, totaling billions of hours each year.
If we had to pay for all that care, it would be worth an astonishing amount of money, far exceeding the revenues of huge companies. This shows the immense contribution of family caregivers.
24. Age of Caregivers
Caregiver age: About 30% of Alzheimer’s/dementia caregivers are age 65 or older themselves. Many caregivers of people with dementia are seniors themselves, often spouses.
This means they’re not only dealing with the challenges of caregiving but also their own aging and health concerns, creating a particularly tough situation.
25. Demographics of Caregivers
Caregiver demographics: Approximately 66% of dementia caregivers are women. In fact, more than one-third of all Alzheimer’s caregivers are daughters caring for their own parent, making middle-aged women a central pillar of the dementia caregiving workforce.
Most dementia caregivers are women, with many being daughters who care for their parents. This highlights the vital role that middle-aged women often play in providing dementia care.
26. Caregiver Burden
Caregiver burden: Caregivers of people with dementia are twice as likely to report substantial emotional, financial, and physical difficulties compared to caregivers of seniors without dementia.
Being a caregiver for someone with dementia can be extremely difficult. These caregivers often face much more stress, financial problems, and physical health issues compared to those caring for seniors without dementia, often leading to higher rates of depression and other health problems.
Caregivers manage a wide range of tasks daily, from personal care to medication reminders. Tools like a caregiver task management list can help manage this demanding role.
27. Caregiving Impact in Massachusetts
Massachusetts caregiving impact: In Massachusetts, about 218,000 family caregivers collectively provided 252 million hours of unpaid care for people with Alzheimer’s and other dementias last year, care valued at approximately $6.7 billion.

Just like the national picture, Massachusetts families provide a huge amount of unpaid care for their loved ones with dementia.
This massive effort, valued in billions of dollars, demonstrates the heavy load carried by families in the state and the impact of dementia prevalence US. While family members provide invaluable unpaid care, exploring professional options can bring different considerations.
Take a closer look at the nuances when seeking private caregiver considerations.
28. Under-Diagnosis of Cognitive Issues
Under-diagnosis of cognitive issues: Only about 1 in 5 U.S. older adults (aged 65–80) reports having undergone any cognitive screening or memory test in the past year.
Even though Medicare covers a yearly check-up that includes a memory test, most older adults in the U.S. aren’t getting screened for problems. This means many cases of dementia might be missed or diagnosed later than they should be.
29. Delays in Diagnosis
Diagnosis delays: The time from the onset of dementia symptoms to an official diagnosis averages around 31 months for White Americans. For Black Americans, the average diagnostic delay is ~35 months, and for Hispanic Americans it is ~44 months. It often takes a long time from when dementia symptoms first appear until a person gets a formal diagnosis.
These delays are even longer for Black and Hispanic Americans, meaning many people, especially in minority communities, are already in the moderate to late stages of dementia by the time they receive a diagnosis.
30. Reactive Doctor Detection
Reactive detection by doctors: Nearly 97% of primary care physicians admit they wait for patients or family members to mention memory/cognitive concerns, rather than proactively screening for dementia. Most doctors wait for patients or their families to bring up memory problems instead of actively looking for signs of dementia.
This approach can lead to diagnoses being missed or happening much later, as many people don’t talk about their cognitive issues until symptoms significantly worsen. The terms ‘home care’ and ‘home health care’ are often used interchangeably, but they refer to distinct types of services.
A clear definition of care type distinctions proves key when planning for a loved one’s needs. Beyond nursing homes, many families weigh the benefits of in-home support versus residential facilities.
Each option has unique advantages, and considering home vs facility care helps families choose wisely. Beyond direct medical or personal care, companionship plays a vital role in reducing loneliness among seniors.
This type of support focuses on social well-being support. The challenges of high turnover are part of a broader issue affecting the entire industry. This growing deficit directly impacts the availability of essential care, reflecting a larger national caregiver shortage.
For comprehensive home care services and further insights, visit Global One Home Care.
Dr. Ella Njike is the CEO and founder of Global One Home Care Boston, a Boston-based agency providing compassionate in-home support for seniors and individuals with disabilities. With a Doctorate and extensive experience working in the healthcare industry, Dr Ella brings a unique understanding to the challenges families face. He established Global One Home Care to ensure that care extends beyond daily tasks, focusing on building genuine connections and respecting each individual's journey. Dr. Njike is deeply committed to creating an environment where clients feel truly valued and at home.
Contact us
We aim to be an active partner in your care, not to take over. You are the CEO of your care, and we support you in managing it effectively.
Here are some features of our Global One Home Care
- 24/7 access to care
- Customized care plans
- Supervisory visits
- Caregiver introductions
- Nutritional planning
- Respite support
- Companionship
- Mobility assistance
- Durable Medical Equipment recommendations
- Errands and Shopping
- Fall Prevention
- ADLs